Dental Insurance
Cigna Dental Care® Health Maintenance Organization (HMO) Prepaid Plan
 800.997.1617
800.997.1617
24/7
cigna.com/stateoftn
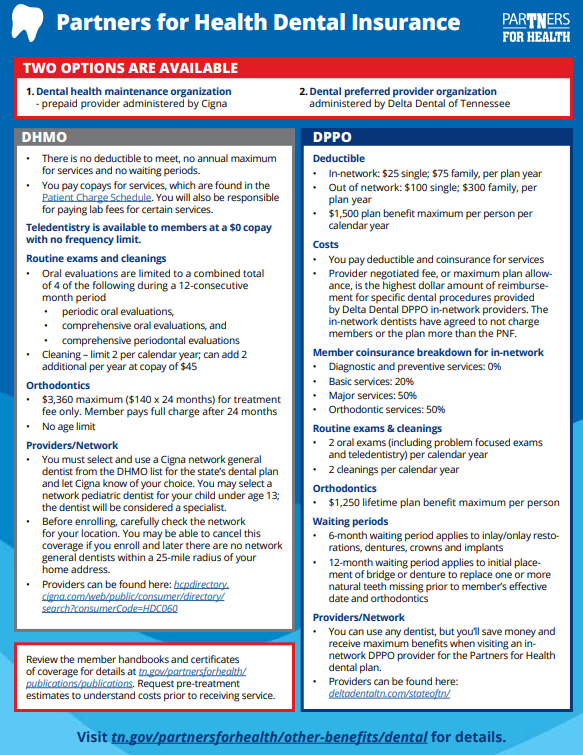
- You must select and use a Cigna network general dentist from the DHMO list for the state’s dental plan and let Cigna know of your choice.
- You must use your selected dentist to receive benefits.
- You may select a network pediatric dentist as the network general dentist for your dependent child under age 13. The pediatric dentist will be considered a “specialist” for plan benefits. At age 13, you must switch the child to a network general dentist or pay the full charge from the pediatric dentist.
- There may be some areas in the state where network general dentists are limited or not available. Before enrolling, carefully check the network for your location.
- With the DHMO, you may be able to cancel this coverage if you enroll and later there are no network general dentists within a 25-mile radius of your home address.
- You pay copays for dental treatments. Review the Patient Charge Schedule under Publications and Dental HMO - Prepaid Provider at https://www.tn.gov/partnersforhealth/publications/publications.html before having procedures performed. Lab fees may apply for some procedures and are the responsibility of the member to pay.
- No deductibles to meet, no claims to file, no waiting periods, no annual dollar maximum.
- Preexisting conditions are covered.
- Referrals to specialists by network general dentists are required.
- Teledentistry is offered at no charge.
- The completion of crowns, bridges, dentures, implants or root canals already in progress on a new member’s effective date will not be covered.
- For orthodontic services in progress, members should contact Cigna customer service for additional information regarding their benefit.
- See the Certificate of Coverage under Publications and Dental HMO - Prepaid Provider at https://www.tn.gov/partnersforhealth/publications/publications.html for complete details.
- To learn about all DHMO benefits, find the Cigna DHMO handbook by clicking on Publications and Dental HMO – Prepaid Provider.
- Search for a provider

800.552.2498
7 a.m. to 5 p.m. CT
DeltaDentalTN.com/StateofTN
- You can use any dentist, but you’ll save money and receive maximum benefits when visiting an in-network DPPO provider for the state's dental plan.
- You pay deductibles and coinsurance for some dental care. Deductible does not apply to diagnostic and preventive benefits such as periodic oral evaluation.
- You or your dentist will file claims for covered services. Discuss any estimated expenses with your dentist or specialist. Your dentist and you may want to request a pre-treatment cost estimate from Delta Dental for some procedures. Charges for dental procedures are subject to change.
- There is a six‐month waiting period from the member’s coverage start date that applies to inlay/onlay, restorations, dentures, crowns and implants. There is a 12-month waiting period from the member’s coverage start date that applies to initial placement of bridge or dentures to replace one or more natural teeth if the tooth or teeth were missing prior to the member's effective date of coverage and for orthodontic treatment.
- Teledentistry is offered and claims are handled as if the patient received dental services in a dental office. Charges are considered as Type A: Diagnostic and Preventive and are subject to frequency limitations.
- Referrals to specialists are not required.
- For orthodontic claims in progress at the time of the member’s effective date, you can ask your orthodontist or dental office to submit a claim with the total fee, initial banding date and total number of months of treatment. This detail will allow Delta Dental to calculate what may be paid.
- See the Certificate of Coverage for coverage details.
- You pay coinsurance for many covered services and your share is based on the provider negotiated fee (PNF) agreed upon by the provider and Delta Dental of Tennessee. The PNF, also called the maximum plan allowance, is the highest dollar amount of reimbursement for specific dental procedures provided by Delta Dental DPPO in-network providers. The in-network dentists have agreed not to charge members or the plan more than the PNF. When a member receives dental services from an out-of-network provider, the out-of-network dentist will be paid by the plan for covered procedures according to the average PNF for in-network providers and respective plan coinsurance. The member is then responsible for all other charges by the out-of-network dentist.
- To learn about all DPPO benefits, find the Delta Dental DPPO handbook under Publications and Dental PPO.
- Search for a provider - Delta Dental DPPO – DeltaDentalTN.com/StateofTN; First, click “Find a Dentist.” Then, select the specialty of providers that you are interested in searching. Please make sure that “Delta Dental PPO” is the selected network option.